As Alzheimer’s disease now affects seven million Americans — the largest number ever — there is a growing demand for new treatments.
Scientists at the University of California, Irvine, have discovered a "groundbreaking" new therapy to fight the disease.
The treatment involves using stem cells to "program" human immune cells, called microglia, to counteract signs of dementia in the brain, according to a press release from UCI.
ALZHEIMER'S RATES HAVE REACHED STAGGERING NUMBER AS EXPERTS CALL FOR CHANGE
Microglia are immune cells found in the central nervous system that act as the brain’s "primary line of defense against infection and injury," according to the reseachers.
Using CRISPR gene editing, the scientists engineered the cells to produce an enzyme called neprilysin, which has been shown to break down the toxic beta-amyloid plaques that build up in the brains of Alzheimer’s patients.

As Alzheimer’s disease now affects seven million Americans — the largest number ever — there is a growing demand for new treatments. (iStock)
In the brains of mice, the engineered cells were found to preserve neurons, decrease inflammation, reduce beta-amyloid build-up and reverse neurodegeneration, the researchers found.
The study, which was funded by the National Institutes of Health, was published in the journal Cell Stem Cell.
'I'M A NEUROLOGIST — HERE'S WHY DEMENTIA IS RISING AND HOW TO REDUCE YOUR RISK’
"Delivering biologics to the brain has long been a major challenge because of the blood-brain barrier," said co-author Mathew Blurton-Jones, professor of neurobiology and behavior, in the release.
"We’ve developed a programmable, living delivery system that gets around that problem by residing in the brain itself and responding only when and where it’s needed."
The programmed cells only target amyloid plaques, researchers noted, which makes the approach "highly targeted yet broadly effective."
"We’ve developed a programmable, living delivery system that gets around that problem by residing in the brain itself and responding only when and where it’s needed."
The study also found that microglia could be effective in combating other central nervous system disorders, such as brain cancer and multiple sclerosis.
"This work opens the door to a completely new class of brain therapies," said Robert C. Spitale, professor of pharmaceutical sciences, in the release.
"Instead of using synthetic drugs or viral vectors, we’re enlisting the brain’s immune cells as precision delivery vehicles."

Using CRISPR gene editing, the scientists engineered the cells to produce an enzyme called neprilysin, which has been shown to break down the toxic beta-amyloid plaques that build up in the brains of Alzheimer’s patients. (iStock)
Dr. Joel Salinas, a behavioral neurologist and associate professor at NYU Grossman School of Medicine, said this study is an "impressive proof of concept" for a highly targeted and responsive brain therapy.
"One of the most exciting aspects is the precision — instead of releasing treatment throughout the brain, these modified cells activate only where disease-related damage is happening," Salinas, who was not involved in the research, told Fox News Digital.
BLOOD PRESSURE AND DEMENTIA RISK SHARE SURPRISING LINK, STUDY SUGGESTS
"That kind of targeted action could help limit harm to healthy brain tissue, reduce side effects, and concentrate therapeutic effects where they are most needed."
While the results are still early and limited to mice, Salinas noted that this strategy opens a "promising new avenue."

While the results are still early and limited to mice, the strategy opens a "promising new avenue," a neurologist noted. (iStock)
Looking ahead, the researchers aim to conduct human trials, potentially using stem cells from each individual patient to reduce the risk of immune rejection, according to the release.
"If future studies show that this approach is safe, durable and effective in humans, it could potentially be adapted not just for Alzheimer’s, but also for other conditions where disease processes are patchy or localized, like brain tumors, multiple sclerosis or other neurodegenerative diseases that cause dementia," Salinas said.
CLICK HERE TO GET THE FOX NEWS APP
Courtney Kloske, Ph.D., director of scientific engagement at the Alzheimer’s Association in Chicago, also reviewed UCI’s study findings.
"With the continued aging of the population, strategic research funding to broaden the therapeutic pipeline for Alzheimer’s and other diseases that cause dementia is critical," she told Fox News Digital.
CLICK HERE TO SIGN UP FOR OUR HEALTH NEWSLETTER
"It’s equally important to explore different drug delivery methods, such as using genetically modified cells as demonstrated in this newly published research."
Kloske noted that these findings are promising and hopeful, but preliminary.

"Additional research is needed to determine how this type of drug delivery mechanism could impact individuals living with or at risk for Alzheimer’s," noted a representative from the Alzheimer’s Association. (iStock)
"Additional research is needed to determine how this type of drug delivery mechanism could impact individuals living with or at risk for Alzheimer’s," she said.
"This work was done in animal models; the authors emphasize the importance of advancing this research into clinical trials in people to better understand the therapeutic potential of this drug delivery mechanism."
For more Health articles, visit www.foxnews.com/health
In addition to the NIH, the study received support from the California Institute for Regenerative Medicine and the Cure Alzheimer’s Fund.
Melissa Rudy is senior health editor and a member of the lifestyle team at Fox News Digital. Story tips can be sent to melissa.rudy@fox.com.
.png)
 German (DE)
German (DE)  English (US)
English (US)  Spanish (ES)
Spanish (ES)  French (FR)
French (FR)  Hindi (IN)
Hindi (IN)  Italian (IT)
Italian (IT)  Russian (RU)
Russian (RU) 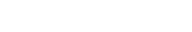 6 hours ago
1
6 hours ago
1




Comments